
September 16, 2025
Salk Institute and UC San Diego scientists find a cell surface sugar that slows pancreatic cancer in mice—and is detectable in patient blood samples
Salk Institute and UC San Diego scientists find a cell surface sugar that slows pancreatic cancer in mice—and is detectable in patient blood samples
LA JOLLA—Pancreatic cancer has the highest mortality rate of all major cancers, and its incidence is climbing. Because it is typically asymptomatic at early stages, pancreatic cancer is especially difficult to catch and treat in time. This allows the cancer to spread or metastasize throughout the body—the ultimate cause of death for nearly all patients.
A new study from the Salk Institute and the University of California San Diego has identified a unique sugar called HSAT (antithrombin-binding heparan sulfate) as a potential therapeutic target for slowing tumor progression and metastasis in pancreatic ductal adenocarcinoma, the most common pancreatic cancer.
The data collected from patient and mouse samples suggest that HSAT is expressed by cells in the pancreas, more so in the early stages and dropping in later stages of cancer progression. This loss prompts increased inflammation and a greater risk of metastasis. The researchers say boosting HSAT may therefore slow the formation and spread of pancreatic cancer. Indeed, patients with higher pancreatic HSAT levels were found to have better survival rates.
The study also found that HSAT was detectable in cancer patients’ plasma, making it potentially useful as a biomarker to help catch and track pancreatic cancer. The findings were published in the Journal of Clinical Investigation on September 16, 2025.
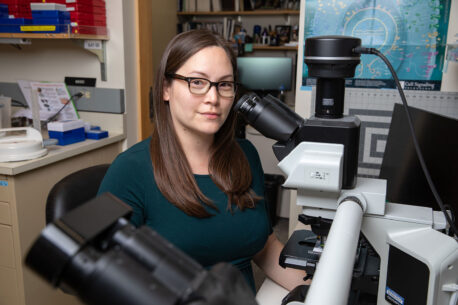
“We need to improve our understanding of the basic biology of pancreatic cancer if we want to one day prevent or cure it, and that’s what we’ve done here,” says co-senior author Dannielle Engle, assistant professor and holder of the Helen McLoraine Developmental Chair at Salk. “We discovered that HSAT is actually much more prevalent in the body than was previously understood, especially in cancer, and that it plays an important role in protecting against pancreatic cancer progression.”
The making of a pancreatic cancer cell
Cancerous cells don’t just appear out of thin air. Rather, they appear when normal cells mutate and begin replicating out of control until a tumor forms. Part of this identity shift from normal to cancerous takes place on the cell’s surface, which is decorated with molecules that mediate the cell’s many interactions with the surrounding cellular world.
Some of these surface molecules are sugars. As these sugars change, so too does the cell’s ability to multiply, migrate, and invade other parts of the body. In fact, this shift in cell surface sugars is one of the reasons pancreatic cancer is so difficult to treat. Pancreatic cancer cells cover themselves with excessive surface sugars—like heparan sulfate—to shield themselves from the immune system and, relatedly, anti-cancer immunotherapies.
To further unpack the relationship between cancer and cell surface sugars, Engle, an expert on pancreatic cancer, forged a partnership with sugar biology experts at UC San Diego. Together, they asked: How might changes to a cell’s surface sugars impact pancreatic cancer progression?
Connecting blood clots and cancer cells
Their question also speaks to a relationship between cardiovascular health and pancreatic cancer. Blood clotting is largely controlled by a protein called antithrombin. To activate antithrombin, the protein must interact with a special form of heparan sulfate, called HSAT.
This same interaction is used to create heparin, which is a form of heparan sulfate that carries the HSAT modification and is used therapeutically by doctors. Anticoagulant drugs are especially important in cancer, since cancer often comes with an elevated risk of blood clots or stroke. HSAT is the body’s own form of heparin, so creating more HSAT could mean less clotting risk for these vulnerable patients.
“Prior to our study, scientists thought HSAT was quite rare in the body. But we observed that pancreatic ductal adenocarcinoma cells express a high level of a key protein involved in forming HSAT, so we thought perhaps these tumors would express HSAT and set out to determine if that was true,” says study first and co-corresponding author Thomas Mandel Clausen, an associate research scientist at UC San Diego at the time of the study. “Very surprisingly, we found HSAT to be abundant in epithelial cells in multiple organs, and that indeed, HSAT was abundant in pancreatic ductal adenocarcinoma—especially in early stages of the disease.”
HSAT protects against pancreatic cancer progression
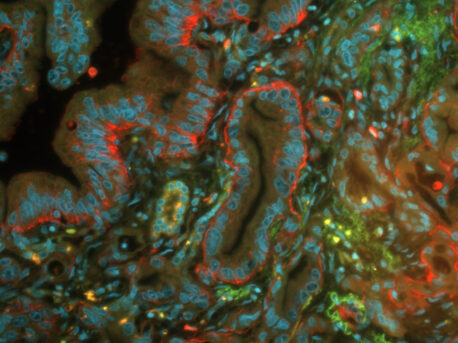
While investigating human pancreatic tissue samples and larger pancreatic cancer databases, the scientists were surprised to find that HSAT was present in both healthy pancreatic tissues and in pancreatic ductal adenocarcinoma. Importantly, patients with more HSAT in their tumors appeared to live longer, suggesting that the molecule may play a protective role in pancreatic cancer.
To explore this possibility further, the researchers developed a mouse model of pancreatic ductal adenocarcinoma. They immediately found HSAT expressed across multiple organs—from the pancreas to the bladder to the lungs—overturning the assumption that HSAT is rare in the body.
The researchers then discovered that pancreatic HSAT levels were especially high in early precancerous lesions and dipped as the cancer progressed. To better understand the molecule’s role here, they blocked HSAT and observed its effect on cancer progression. In mice growing tumors with no HSAT, pancreatic tumors were more inflamed, more resistant to cell death, and twice as likely to metastasize. The findings suggest that HSAT plays a critical role in suppressing the formation and spread of pancreatic tumors—a function that could potentially be enhanced to help treat the disease.
Additional experiments showed that HSAT’s protective properties may stem from its regulation of the thrombin/PAR-1 axis, which mediates the interplay between blood coagulation and inflammation. Continued exploration of this molecular pathway will be critical for future drug development.
“An intervention that increases heparan sulfate levels to produce more HSAT could be an effective way to both reduce blood clots and slow cancer metastasis,” Engle says.
A new biomarker and therapeutic target
The study is the first to demonstrate that HSAT is abundant in epithelial cells throughout the body, and that HSAT loss can make pancreatic cancer more difficult to kill and more likely to spread. Furthermore, seeing HSAT expressed in other organs suggests that a similar mechanism may exist in other cancers.
In addition to being a promising potential therapeutic target, HSAT may also serve as a useful biomarker of pancreatic cancer. The researchers confirmed that HSAT can be detected in human plasma samples, and that HSAT levels are correlated with distinct tumor stages, meaning the molecule could be used to help diagnose and continually stage pancreatic cancer progression.
“The clinical application of our findings remains to be determined, but the implication is that patients expressing higher levels of HSAT may live longer,” says co-senior author Jeffrey Esko, distinguished professor and founding co-director of the Glycobiology Research and Training Center at UC San Diego. “If we can find ways to increase HSAT expression or screen for HSAT levels in patients, we could potentially alter the mortality outcomes for pancreatic cancer by catching it earlier and treating it more effectively.”
Other authors include Jacob Tremblay, Hyemin Song, Kristina Peck, and Satoshi Ogawa of Salk; Ryan Weiss of UC San Diego and University of Georgia; Benjamin Kellman of Ragon Institute; Joanna Coker of UC San Diego and Brown University; Leo Dworkin, Jessica Perez-Ochoa, Ivy Chang, Timothy Chen, Vikram Padala, Daniel Sandoval, Maike Sander, Dzung Le, and Nathan Lewis of UC San Diego; Richard Karlsson, Hiren Joshi, and Rebecca Miller of University of Copenhagen; Gaowei Wang of Sanford Consortium for Regenerative Medicine; L. Paige Ferguson of UC San Diego and Cold Spring Harbor Laboratory; Nikita Bhalerao of University of Massachusetts; Allison Moores of Bishops School; Tannishtha Reya of UC San Diego and Columbia University; Thomas Caffrey, Jean Grem, Michael Hollingsworth, and Paul Grandgenett of University of Nebraska; Alexandra Aicher of China Medical University; Christopher Heeschen of Candiolo Cancer Institute; Susan Bellis of University of Alabama; Mark Fuster of VA San Diego Healthcare System and UC San Diego; and David Dawson of UC Los Angeles.
The work was supported by the Cancer Research Coordinating Committee (C23CR5578), National Institutes of Health (NHLBI HL131474, NIGMS GM150736, NHLBI HL167091, NCI CA197699, T32 GM007752, NIGMS GM119850, NCI CA211462, NCI U01 CA233581, P30 CA23100, S10 OD026929), Alfred Benzon Foundation, Dagmar Marshall Foundation, Novo Nordisk Foundation (NNF22OC0076899, NNF22OC0073736), Ruth L. Kirschstein National Research Service Award (F31 CA247489), and U.S. Department of Veterans Affairs Merit Award (I01-BX003688-05A2).
DOI: 10.1172/JCI184172
JOURNAL
Journal of Clinical Investigation
AUTHORS
Thomas Mandel Clausen, Ryan J. Weiss, Jacob R. Tremblay, Benjamin P. Kellman, Joanna Coker, Leo Dworkin, Jessica Perez-Ochoa, Ivy Chang, Timothy Chen, Vikram Padala, Richard Karlsson, Hyemin Song, Kristina Peck, Satoshi Ogawa, Daniel R. Sandoval, Hiren J. Joshi, Gaowei Wang, L. Paige Ferguson, Nikita Bhalerao, Allison Moores, Tannishtha Reya, Maike Sander, Thomas C. Caffrey, Jean L. Grem, Alexandra Aicher, Christopher Heeschen, Dzung Le, Nathan E. Lewis, Michael A. Hollingsworth, Paul M. Grandgenett, Susan L. Bellis, Rebecca Miller, Mark M. Fuster, David W. Dawson, Dannielle D. Engle, and Jeffrey D. Esko
Office of Communications
Tel: (858) 453-4100
press@salk.edu
The Salk Institute is an independent, nonprofit research institute founded in 1960 by Jonas Salk, developer of the first safe and effective polio vaccine. The Institute’s mission is to drive foundational, collaborative, risk-taking research that addresses society’s most pressing challenges, including cancer, Alzheimer’s, and agricultural resilience. This foundational science underpins all translational efforts, generating insights that enable new medicines and innovations worldwide.