
July 29, 2025
Salk researchers find immune cells travel from the gut to the mammary gland to support lactation
Salk researchers find immune cells travel from the gut to the mammary gland to support lactation
LA JOLLA—Of the 3.6 million babies born in the United States each year, around 80 percent begin breastfeeding in their first month of life. Breastfeeding has known benefits for both mother and child, reducing maternal risk of breast and ovarian cancers, type 2 diabetes, and high blood pressure, while simultaneously supporting the baby’s nutrition and immune system. But because pregnancy and lactation have been historically understudied, we still don’t understand the science behind many of these benefits.
Salk Institute immunologists are changing that—starting with a map of immune cell migration before and during lactation. Using both animal research and human milk and tissue samples, the researchers discovered that immune cells called T cells are abundant in the mammary glands during pregnancy and breastfeeding, with some relocating from the gut. These cells likely support both maternal and infant health.
The findings, published in Nature Immunology on July 29, 2025, may help explain the advantages of breastfeeding, prompt new solutions for mothers unable to breastfeed, and inform dietary decisions that enhance breast milk production and quality.
“By investigating how immune cells change during pregnancy and lactation, we were able to find lots of exciting things—notably, that there’s a significant increase in immune cells in mammary tissue during lactation, and the increase in immune cells requires microbes,” says Assistant Professor Deepshika Ramanan, senior author of the study.
What we know: Babies get gut bacteria and antibodies from mother’s milk
Most breastfeeding studies focus on the relationship between milk content and infant health. These studies, including previous work by Ramanan, have shown that babies receive important gut bacteria and antibodies from their mother through the breast milk, which lays a critical foundation for their developing immune system. Still, much less is known about the changes to the mother’s body during this time.
Some features of the mammary gland immune landscape can be inferred from milk content research. For example, the presence of antibodies in breast milk means that antibody-producing immune cells called B cells must be present. But few have looked directly at immune cell activity within the mammary gland itself.
What’s new: Mom’s gut microbes boost immune cells in mammary glands
“What’s really exciting is that we didn’t just find more T cells in mammary glands, we found that some of these T cells were actually coming from the gut,” says first author Abigail Jaquish, a graduate student researcher in Ramanan’s lab. “We think they are likely supporting mammary tissue in the same way they typically support intestinal tissue.”
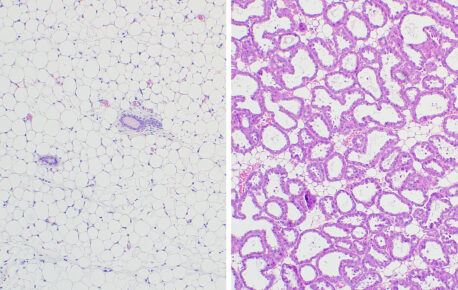
The researchers began their study by looking at mouse mammary gland tissues at various stages pre- to post-lactation. By comparing these samples, they discovered that three different types of T cells were growing in number: CD4+, CD8αα+, and CD8αβ+ T cells.
This was curious to the team, because these T cell subtypes are members of a special immune cell class called intraepithelial lymphocytes. Intraepithelial lymphocytes live in mucosal tissues—soft tissues like the intestines or lungs that are exposed to substances from the outside world. Because these tissues are more vulnerable, intraepithelial lymphocytes act as “resident” immune cells, stationed on-site and ready for action.
The researchers noticed these CD4+, CD8αα+, and CD8αβ+ T cells were lining the mammary epithelium the same way they would line the epithelium of other mucosal tissues. What’s more, these T cell subtypes bore gut-resident surface protein fingerprints—pointing to T cell migration between the intestines and mammary glands. Together, these changes were facilitating a mammary gland transition from non-mucosal to mucosal tissue in preparation for lactation, where it would become exposed to the outside environment, including microbes from the mother’s skin and the infant’s mouth.
But was this also happening in humans? An investigation into databases of human breast tissue and milk samples from the Human Milk Institute at UC San Diego revealed yes—human equivalents of these intraepithelial lymphocytes showed the same trends.
The team returned to the mouse model with one final question: Are these mammary gland T cells impacted by microbes the same way they would be in the gut? They compared the mammary glands of mice living in normal and germ-free environments and found that all three T cells subtypes were expressed far more in mice exposed to microbes. This finding suggests that maternal microbes modulate the number of T cells created during lactation, which in turn could impact the strength of the mammary gland immune barrier.
Altogether, T cell production ramped up with the help of microbes, T cells relocated from the gut to mammary glands, and the mammary glands switched from non-mucosal to mucosal tissues.
Looking ahead: What affects this gut-breast immune axis, and thus influences our health for generations?
“We now know so much more about how the maternal immune system is changing during this critical time,” says Ramanan, “and we can now use this information to start exploring the direct effects of these immune cells on both maternal and infant health.”
The researchers hypothesize that hormones influence these many changes, and that the overall goal is protecting the mother from the outside world and related infection. But how they influence lactogenesis, milk quality, and maternal and baby health is the next case to crack.
“There’s so much more research to be done in this area—we’re just getting started,” adds Jaquish. “If we’re seeing a connection between the gut and the mammary gland, what other interactions might be happening in the body? And what else could be impacting the milk that we’re passing on to our offspring?”
Understanding maternal immune cell changes during pregnancy and lactation can impact generations, as mother to child immune and microbiome transfers occur again and again. The insights may also lead to solutions for mothers who cannot breastfeed, either with therapies that help support natural milk production or with more sophisticated formulas that provide some of the same immune support. As the connection between the gut and mammary gland becomes clearer, scientists could one day suggest diets to promote mammary and maternal health, as well as optimize milk quality.
Other authors include Eleni Phung and Isabelle Bursulaya of Salk; Xutong Gong, Silvia Galvan-Pena, Ian Magill, Diane Mathis, and Christophe Benoist of Harvard Medical School; Pilar Baldominos, Eleonara Marina, and Judith Agudo of Dana-Farber Cancer Institute; Kerri Bertrand and Christina Chambers of UC San Diego; Andrés R. Muñoz-Rojas of Rensselaer Polytechnic Institute; and ImmgenT consortium members.
The work was supported by the Damon Runyon Dale F. Frey Award, UC San Diego PiBS T32, National Institutes of Health (RO1-AI150686, R24-072073, NCI CCSG P30 CA014195, NIA San Diego Nathan Shock Center P30 AG068635, NCI CCSG: P30 CA01495, S10 OD023689, S10 OD034268), Chapman Foundation, and Helmsley Charitable Trust.
DOI: 10.1038/s41590-025-02218-3
JOURNAL
Nature Immunology
AUTHORS
Abigail Jaquish, Eleni Phung, Xutong Gong, Pilar Baldominos, Silvia Galvan-Pena, Ian Magill, Isabelle Bursulaya, Eleonara Marina, ImmgenT consortium, Kerri Bertrand, Christina Chambers, Andrés R. Muñoz-Rojas, Judith Agudo, Diane Mathis, Christophe Benoist, Deepshika Ramanan
Office of Communications
Tel: (858) 453-4100
press@salk.edu
The Salk Institute is an independent, nonprofit research institute founded in 1960 by Jonas Salk, developer of the first safe and effective polio vaccine. The Institute’s mission is to drive foundational, collaborative, risk-taking research that addresses society’s most pressing challenges, including cancer, Alzheimer’s, and agricultural resilience. This foundational science underpins all translational efforts, generating insights that enable new medicines and innovations worldwide.