
December 6, 2023
Salk researchers discovered that an anti-cancer therapy can prevent the activation of fibroblasts, cells that typically form protective barriers around pancreatic tumors
Salk researchers discovered that an anti-cancer therapy can prevent the activation of fibroblasts, cells that typically form protective barriers around pancreatic tumors
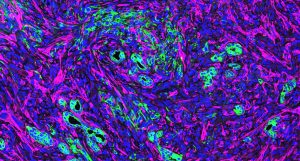
LA JOLLA—Pancreatic cancer is one of the deadliest cancers—only about one in eight patients survives five years after diagnosis. Those dismal statistics are in part due to the thick, nearly impenetrable wall of fibrosis, or scar tissue, that surrounds most pancreatic tumors and makes it hard for drugs to access and destroy the cancer cells.
Now, researchers at the Salk Institute have discovered how a class of anti-cancer drugs called HDAC inhibitors can help treat pancreatic cancer by modulating the activation of fibroblasts—the cells that make up that wall of scar tissue.
The new research was published in Nature Communications on December 6, 2023.
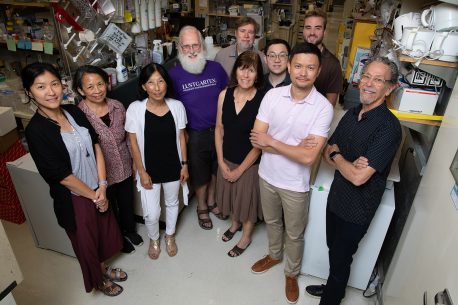
“These drugs turn out to be hitting both the tumor itself as well as the fibrotic tissue around it. This could be a very effective way to treat pancreatic cancers, which have typically been very difficult to reach,” says senior author Professor Ronald Evans, director of Salk’s Gene Expression Laboratory and March of Dimes Chair in Molecular and Developmental Biology.
In response to a new pancreatic tumor, the pancreas typically activates fibroblasts—the connective cells that support the structure of most organs. When flipped from a resting state to an active state, fibroblasts build a thick layer of scar tissue around the cancer. While this normal protective mechanism can help wall off a cancer and prevent its spread, fibroblasts also produce signaling molecules that the tumor itself takes advantage of to grow.
“In the context of most pancreatic cancers, fibroblasts are acting as both good players and bad players,” says Michael Downes, senior staff scientist and co-corresponding author on the paper. “It’s a double-edged sword.”
In the new research, the team probed the effect on fibroblasts of an experimental class of cancer drugs known as histone deacetylase (HDAC) inhibitors. HDACs alter the three-dimensional structure of DNA inside cells, making some stretches of DNA easier or harder for other molecules to access and read. Targeting HDACs can therefore prevent cells from making large changes to their behavior, such as the out-of-control growth of cancer cells. But how the drugs work on all cell types is not well understood.
In experiments on isolated cells, the researchers discovered that HDAC inhibitors prevented fibroblasts from becoming activated and tumor supportive.
“Using HDAC inhibitors actually did two things—it both turned down the growth signals from the fibroblasts to the cancer cells and it reduced the actual activation and accumulation of the fibroblasts,” says Gaoyang Liang, first author and research associate in Evans’ lab.
In mice, the researchers found that one experimental HDAC inhibitor, entinostat, both reduced the activation of fibroblasts around pancreatic tumors and slowed tumor growth. When the researchers analyzed data from humans with pancreatic cancer, they discovered something similar: the higher the levels of HDAC1 in the fibrotic tissue around a patient’s tumor, the worse their outcome.
“This is in agreement with what we saw in cells and in mice,” says Downes. “If you have more HDAC activities in the fibroblasts, you have a worse outcome. On the other hand, if you inhibit the HDACs, you have a better outcome.”
Since HDAC inhibitors work by preventing cells from activating certain genetic programs, the researchers wanted to know which stretches of DNA impacted by the drugs were most relevant for fibroblast activation. They identified several genes that HDAC inhibitors prevent from being expressed—suggesting that new drugs could target those genes to keep fibroblasts from becoming activated and promoting cancer growth and fibrosis.
“There have been some questions in the past about whether targeting fibroblasts is a good thing or a bad thing in pancreatic cancers, because people have shown that if you get rid of fibroblasts altogether it actually makes the cancers more aggressive,” says Annette Atkins, co-author of the study and senior research scientist in Evans’ lab. “But what our results suggest is that we don’t have to get rid of them; just limiting their activation is beneficial.”
More work is needed to pinpoint how to best deliver HDAC inhibitors to the dense fibrotic tissue around pancreatic tumors, as well as how they might be most effectively combined with other cancer treatments.
Other authors of the paper are Tae Gyu Oh, Nasun Hah, Yu Shi, Morgan L. Truitt, Corina E. Antal, Annette R. Atkins, Yuwenbin Li, Antonio F. M. Pinto, Dylan C. Nelson, Gabriela Estepa, Senada Bashi, Ester Banayo, Yang Dai, Ruth T. Yu, Tony Hunter, and Dannielle D. Engle of Salk; Hervé Tiriac of UC San Diego; Cory Fraser of HonorHealth Scottsdale; Serina Ng, Haiyong Han, and Daniel D. Von Hoff of The Translational Genomic Research Institute; and Christopher Liddle of the University of Sydney.
The work was supported by grants from the Lustgarten Foundation (552873, 122215393-02), Don and Lorraine Freeberg Foundation, the David C. Copley Foundation, the Wasily Family Foundation, Ipsen Bioscience, a Stand Up To Cancer-Cancer Research UK-Lustgarten Foundation Pancreatic Cancer Dream Team Research Grant (SU2C-AACR-DT-20-16), the NOMIS Foundation, a Ruth L. Kirschstein National Research Service Award (F32CA217033), a Life Sciences Research Foundation Fellowship, the Damon Runyon Cancer Research Foundation (DRG-2244-16), an Institutional Research Training Grant (5T32CA009370), the National Institutes of Health (CA220468, CA265762, CA082683, 5T32CA009370, NCI CCSG: P30 014195), the Waitt Foundation, and the William Isacoff Research Foundation.
DOI: 10.1038/s41467-023-42178-6
JOURNAL
Nature Communications
AUTHORS
Gaoyang Liang, Tae Gyu Oh, Nasun Hah, Hervé Tiriac, Yu Shi, Morgan L. Truitt, Corina E. Antal, Annette R. Atkins, Yuwenbin Li, Cory Fraser, Serina Ng, Antonio F. M. Pinto, Dylan C. Nelson, Gabriela Estepa, Senada Bashi, Ester Banayo, Yang Dai, Christopher Liddle, Ruth T. Yu, Tony Hunter, Dannielle D. Engle, Haiyong Han, Daniel D. Von Hoff, Michael Downes, Ronald M. Evans
Office of Communications
Tel: (858) 453-4100
press@salk.edu
Unlocking the secrets of life itself is the driving force behind the Salk Institute. Our team of world-class, award-winning scientists pushes the boundaries of knowledge in areas such as neuroscience, cancer research, aging, immunobiology, plant biology, computational biology and more. Founded by Jonas Salk, developer of the first safe and effective polio vaccine, the Institute is an independent, nonprofit research organization and architectural landmark: small by choice, intimate by nature, and fearless in the face of any challenge.